By Doc Willie Ong (Internist and Cardiologist)
Aortic aneurysm is in the news nowadays because of the autopsy findings on Christine Dacera, a 23 year-old flight attendant who died mysteriously. Some people are confused between an aortic aneurysm versus a cerebral or brain aneurysm. Let us learn about aortic aneurysms and how to avoid this.
First of all, both aortic aneurysm and brain aneurysm, refers to a bulging of an artery in the body. However, the location and symptoms are different.
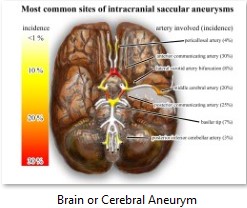
In brain or cerebral aneurysm, there could be severe headache. Around 5 percent of the population has this condition. This occur when the wall of a blood vessel in the brain becomes weakened and bulges or balloons out. Many cases of brain aneurysm are hereditary. Definitive treatment is surgery but there are some cases when medical treatment is preferred.
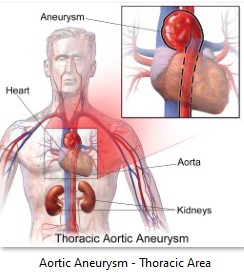
Aortic aneurysm, on the other hand, refers to a bulging in the walls of the aorta. It’s the largest artery in the body, which is around 3 centimeters in diameter. It is shaped like a walking cane, which starts from the heart and goes on a u-turn down to the chest cavity and abdomen area.
The aorta is softer and fleshier in consistency. This is important for it to withstand the powerful surge of blood pumped by the heart. The upper part of the aorta (the “u” part) is called the ascending aorta. The middle part in the chest area is called the thoracic aorta, while the aorta in the abdomen area is called the abdominal aorta.
Depending on which area of the aorta bulges, it is called thoracic aortic aneurysm or abdominal aortic aneurysm.
Aortic Aneurysm: A Serious Condition
If there is too much pressure inside the aorta (like a blood pressure of 180 over 100), the inner part of the aorta (the intima wall) can tear up. Thereby causing the blood to flow through a flap created by the loosening of the inner wall. This condition is known as an aortic dissection, a dangerous situation needing urgent medical and possible surgical treatment.
Different From A Heart Attack:
A common mistake, even by doctors, is to label an aortic dissection as a heart attack. Although the patient may complain of the same back and chest pain, the two diseases are very different.
A heart attack involves a blockage in the small arteries attached to the heart. However, an aortic dissection involves a tear in the wall of the largest artery of the body. In some unfortunate situations, the patient can have both conditions especially if the tear in is the ascending part of the aorta.
Aortic Aneurysm: Who are at risk?
Risk factors for aortic aneurysm and brain aneurysm are similar:
- The elderly – Usually, an aortic dissection does not occur spontaneously. This is brought about by years of wear and tear on the aorta.
- Those with high blood pressure – If the blood pressure is constantly above the upper limit of 140 over 90, this can initially lead to a ballooning of the aorta (called an aortic aneurysm), and later on, to an aortic dissection.
- Those with high cholesterol and smokers.
- Traumatic injuries to the chest or abdomen.
- Drug use such as cocaine and similar drugs – Cocaine causes aneurysms by weakening the inner lining of blood vessels. Cocaine increases blood pressure by tightening blood vessels (vasoconstriction). High blood pressure causes small tears on the inside of blood vessels.
- Hereditary – Inherited connective tissue disorders.
- Family history of aneurysm.
How to detect aortic dissection
The main symptom of a rupture or dissection of the aorta is excruciating pain in the chest or abdominal area. The will depend if the dissection is in the thoracic or abdominal aorta, respectively. Since the aorta supplies the arteries to the arms and legs, the patient may have weak pulses and unequal blood pressures. Dizziness, loss of consciousness, and numbness and paralysis of various parts of the body may also occur.
To diagnose aortic dissection, doctors request for a CT Scan or an MRI of the chest and/or abdomen. If this test is negative, doctors request a more invasive test called an Aortography. Aortography involves inserting a special wire inside the aorta and using contrast dye to detect the dissection.
Treatment of Aortic Dissection:
Treatment of aortic dissection involves two strategies: ggressive medical therapy to lower the blood pressure and possible surgical intervention to repair the defect.
Since the most crucial factor that favors dissection is the blood pressure, doctors prescribe drugs called beta-blockers to decrease the force of the heart’s pumping.
Surgery may be needed in complicated cases, such as blockage in the arteries of the limbs, persistent pain, and ballooning of the aorta with danger of a full-blown rupture. That is why this condition is sometimes called a ‘walking time bomb’ since we don’t know when the rupture will occur.
Dissecting aorta by the numbers:
Since no one can determine when a dissecting aorta will happen, doctors rely on data showing the percentages of such occurrence.
Around 1 in 5 patients with aortic dissection die before reaching the hospital. Without treatment, the mortality rate is 25% in one day; 50% in one week, 75% in one month, and 90% in three months.
When the patient reaches the hospital, the mortality rate is about 30% for a dissection of the ascending and thoracic aorta; and 10% for the abdominal aorta.
For the patients who survive the acute episode, survival rate is around 60% in 5 years and 40% in 10 years.
The most important late complications are redissection and formation of a localized weakness in the aorta. These conditions are serious and may need surgical repair.